In the aftermath of global crises like the COVID-19 pandemic, the healthcare industry has faced a harsh reckoning with the fragility of its supply chains, prompting health systems to impose increasingly stringent demands for resilience, which may be creating more problems than they solve. These efforts, often embedded in detailed Requests for Proposals (RFPs), are designed to secure a steady flow of critical medical supplies and protect patient care from disruptions. However, a growing concern has emerged that such rigorous standards might burden suppliers with unsustainable costs and risks while potentially undermining the very goals they aim to achieve. As health systems push for greater transparency and risk management, the unintended consequences—ranging from market exclusion to inflated expenses—raise questions about whether this aggressive pursuit of stability is inadvertently destabilizing the ecosystem. This complex dynamic demands a closer look at the balance between preparedness and practicality in healthcare supply chain management.
The Fragility of Healthcare Supply Chains
Historical Cost Focus and Vulnerability
The healthcare industry’s long-standing obsession with cost efficiency has shaped supply chains into lean, global networks that prioritize savings over robustness, leaving them alarmingly susceptible to unexpected disruptions. For decades, health systems have streamlined operations by outsourcing production to low-cost regions and minimizing inventory to reduce overhead. While this approach thrived in stable conditions, it crumbled under the strain of crises like the COVID-19 pandemic, exposing a critical lack of resilience. The drive for cheaper supplies often meant sacrificing redundancy and local sourcing, which are vital buffers against sudden shocks. As a result, when demand surged or logistics faltered, hospitals faced dire shortages of essential items like masks and ventilators. This historical focus on trimming expenses has created a system where efficiency comes at the expense of preparedness, revealing a fundamental flaw in how healthcare supply chains have been structured to handle rare but devastating events.
A deeper examination of this vulnerability shows that the globalization of supply chains, while cost-effective, often involves intricate dependencies on distant manufacturers and limited visibility into secondary suppliers. When a single link in this chain breaks—whether due to geopolitical tensions, natural disasters, or pandemics—the ripple effects can paralyze entire systems. Health systems, under constant financial pressure, have historically resisted investing in backup plans or diversified sourcing, viewing such measures as unnecessary expenses. Yet, the cost of inaction has proven far greater, with disruptions leading to delayed treatments and compromised care. The lesson is stark: a supply chain optimized solely for cost leaves little room for error when the unexpected strikes. Moving forward, acknowledging this trade-off between savings and stability is essential to rebuilding a framework that can endure unforeseen challenges without sacrificing patient safety.
Lessons from Disruptions
The real-world impact of supply chain fragility became painfully clear during the COVID-19 crisis, when shortages and backorders of critical medical supplies disrupted hospital operations on an unprecedented scale. Items as basic as personal protective equipment and as complex as ventilators became scarce, forcing healthcare providers to ration resources and delay non-emergency procedures. This not only strained hospital staff but also directly affected patient outcomes, with some facilities unable to provide timely care due to missing equipment. The cascading effect of these shortages highlighted how deeply interconnected and vulnerable the supply network had become, with even minor delays in one region causing major setbacks across continents. Such disruptions underscored the urgent need for a shift in priorities, pushing health systems to rethink their approach to supply chain management and focus on building resilience against future crises.
Beyond the immediate operational challenges, these disruptions exposed systemic weaknesses that have long been ignored in the pursuit of cost-cutting. Hospitals found themselves competing for limited supplies, driving up prices and exacerbating inequities in access to care. Smaller facilities, lacking the purchasing power of larger systems, often fared worst, unable to secure essentials during peak demand. The fallout extended to patient trust, as public confidence in healthcare’s ability to respond to emergencies wavered. These lessons have fueled a broader recognition that resilience must be a cornerstone of supply chain strategy, not an afterthought. However, addressing this need requires more than reactive measures; it demands a fundamental reevaluation of how health systems balance financial constraints with the imperative to maintain uninterrupted access to life-saving resources in times of crisis.
The Burden of Escalating Resilience Standards
Challenges for Suppliers
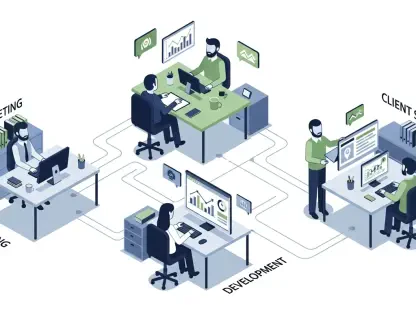
As health systems respond to past disruptions by tightening supply chain requirements, suppliers face an uphill battle to meet the complex demands outlined in modern RFPs, often at the expense of their operational capacity. These standards frequently mandate detailed mapping of secondary and tertiary supply chains, alongside sophisticated risk monitoring and demand management practices. For small suppliers, the resource burden is overwhelming, as they lack the staff, technology, or capital to comply with such intricate expectations. This creates a barrier to entry, effectively sidelining smaller players who might otherwise offer competitive pricing or niche innovations. The push for resilience, while well-intentioned, risks shrinking the supplier pool, reducing diversity in the market, and potentially driving up costs for health systems that rely on a broader range of vendors to maintain affordability.
Large suppliers, though better equipped, are not immune to the challenges posed by these escalating standards, as the sheer scale of their product portfolios complicates compliance efforts. Managing thousands of items across global networks requires significant investment in data systems and personnel to track and report on every layer of the supply chain. This diverts resources from core activities like product development or quality assurance, potentially stifling innovation. Furthermore, the administrative burden of meeting RFP criteria can shift focus from delivering value to simply checking boxes, creating inefficiencies that ripple through the industry. The disparity in how these demands affect suppliers of different sizes highlights a critical flaw in the current approach: resilience standards, if not carefully calibrated, may punish rather than protect, undermining the collaborative relationships needed to strengthen the supply chain as a whole.
Operational and Financial Consequences
The operational toll of complying with heightened resilience standards is substantial, as suppliers must overhaul processes and invest heavily in systems to align with health systems’ expectations, often at a significant cost. Implementing advanced tracking tools, hiring additional staff for risk assessment, and maintaining detailed documentation require financial outlays that many suppliers struggle to absorb. These expenses inevitably trickle down, either through higher prices for medical supplies or reduced profit margins that threaten long-term sustainability. For health systems already grappling with tight budgets, this cost escalation poses a dilemmthe pursuit of a more robust supply chain may inadvertently strain the very financial resources needed to deliver patient care. The irony is evident—efforts to prevent disruptions could create new economic pressures that hinder healthcare delivery.
Equally concerning are the business risks tied to the transparency demanded by these standards, particularly the requirement to disclose proprietary information about supply chain mappings and continuity plans. Sharing such sensitive data opens suppliers to potential competitive harm, as rivals or other entities could exploit this insight to undercut pricing or disrupt partnerships. The fear of intellectual property exposure adds a layer of reluctance, with some suppliers opting to withdraw from bidding processes rather than risk their strategic advantage. This dynamic not only limits the pool of willing participants but also fosters distrust between health systems and suppliers, complicating efforts to build a cohesive, resilient network. Addressing these operational and financial consequences requires a nuanced approach that safeguards sensitive information while still ensuring accountability, a balance that current standards often fail to strike.
Unintended Outcomes of Stringent Demands
Market Exclusion and Skewed Priorities
The aggressive push for supply chain resilience through rigid standards is inadvertently reshaping the healthcare supplier landscape, often excluding capable vendors who cannot meet the stringent criteria set forth in RFPs. Small and medium-sized suppliers, despite offering quality products or innovative solutions, frequently lack the infrastructure to document extensive risk management plans or map out every tier of their supply network. This exclusion narrows the competitive field, favoring larger entities with deeper resources, even if their offerings are not always the most cost-effective or superior in quality. Such a trend risks creating a less dynamic market, where health systems have fewer options and face higher costs due to reduced competition. Ultimately, this shift could compromise the affordability and diversity of medical supplies, counteracting the goal of ensuring consistent access for patient care.
Moreover, the emphasis on compliance over substance in supplier selection processes threatens to skew priorities away from what truly matters—delivering value and improving patient outcomes. Health systems may gravitate toward vendors who excel at meeting bureaucratic benchmarks rather than those who provide the best products at reasonable prices. This misalignment can stifle innovation, as suppliers focus on ticking boxes rather than investing in research or development. The ripple effect extends to patients, who may face delays or higher costs for treatments if the market prioritizes paperwork over performance. Recognizing this unintended consequence is crucial, as it highlights how resilience standards, if overly rigid, can distort the very principles they aim to uphold, pushing health systems to reconsider how they evaluate and partner with suppliers in a rapidly evolving landscape.
The Need for Balance
Achieving a resilient healthcare supply chain hinges on shared responsibility, requiring both health systems and suppliers to move beyond past cost-driven practices and collaborate on standards that are practical and equitable. Both parties have historically contributed to the fragility of the current system by prioritizing short-term savings over long-term stability, a mindset that must shift to prevent future crises. Health systems should ease the burden of overly complex requirements, focusing instead on core resilience metrics that do not disproportionately disadvantage smaller players or inflate costs. Meanwhile, suppliers must commit to transparency and proactive risk management within reasonable limits. This mutual accountability can foster trust, ensuring that efforts to strengthen supply chains do not create new barriers but rather build a foundation for sustainable reliability.
Looking back, the journey to balance was marked by a necessary reckoning with the limitations of past strategies, as both sides grappled with the fallout of disruptions that exposed deep vulnerabilities. The dialogue that emerged from those challenges laid the groundwork for compromise, with early steps toward more tailored resilience frameworks showing promise. Moving forward, the focus should be on actionable solutions—such as joint risk assessments or tiered compliance models—that accommodate diverse supplier capabilities while safeguarding patient care. Additionally, investing in technology to streamline transparency without compromising competitive edges could prove transformative. By reflecting on lessons learned and prioritizing collaboration over confrontation, health systems and suppliers can chart a path that not only mitigates risks but also preserves the affordability and accessibility essential to effective healthcare delivery.